Hospital and medical facility managers recognize EMR systems as a necessary part of managing patient medical data. In an increasingly digital world, more and more records are stored electronically, while paper records storage systems move further into obsolescence.
But even as EMR systems become ubiquitous in health information management, challenges surround their use and implementation as well. EMR systems represent expensive investments upfront and can be costly to manage over time. They draw on hospital resources directly, through items like software licensing fees, and indirectly, by diverting employee productivity and energy away from patient outcomes.
This is especially true for hospitals and facilities undergoing mergers or acquisitions of new facilities. Hospitals in such situations often find themselves acquiring and managing multiple EMR systems across old and newly acquired branches as they inherent legacy systems from newly acquired hospitals and hospital systems. This creates inefficiency, and targeting those inefficiencies represents an opportunity to reduce expenses and capture savings.
The Problem
The challenges hospital systems and organizations face in transition are straightforward. First, managing newly acquired record sets from separate EMR systems is never as simple as plugging all the new records into your facility’s legacy system, yet keeping surplus EMR software online to store newly acquired record sets is a recipe for inefficiency. This means holding onto multiple systems often seems like the only reasonable option, so many hospitals take on the hidden cost of inefficient EMR system management, like excessive licensing fees and sapped employee productivity, without even realizing it.
For any EMR system, whether newly implemented or newly acquired, there are steps that can make implementing and operating the system seamless and successful, helping to avoid the kind of inefficient processes that create revenue drains within health information management departments. Unfortunately, when a hospital acquires a preexisting EMR system through merger or acquisition, they have little choice over how it was implemented or how it’s managed in the present day. The software itself used in an acquired facility may be different than the one used by the acquiring facility, while the processes used to employ the software may be different entirely than typical processes at the acquiring facility.
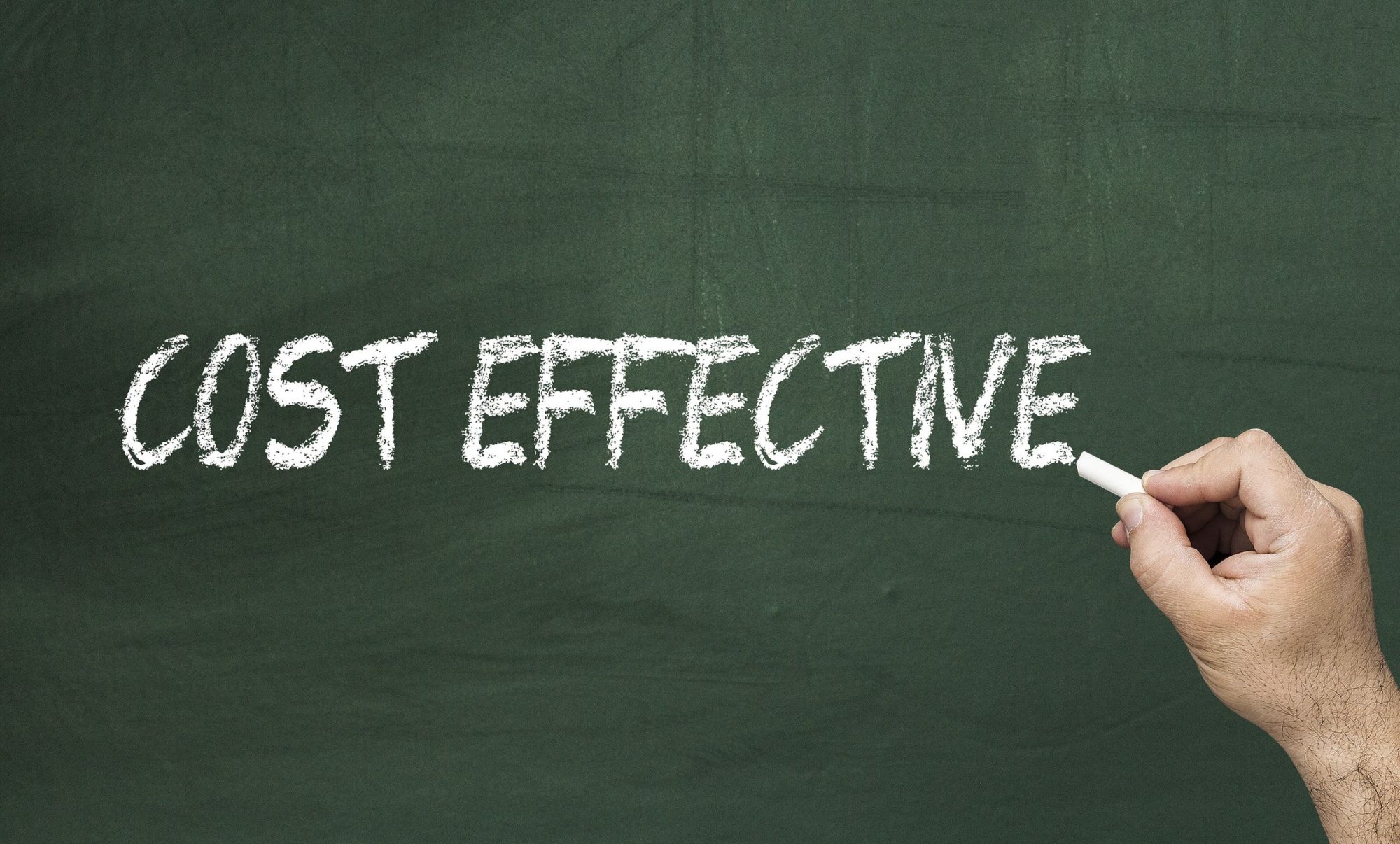
To understand how the problem can look in real terms, consider this example: A hospital network with several branches manages their records using the same EMR system across all branches of the network. In the space of five years, this hospital acquires two separate facilities. With the acquisition of these facilities, the purchasing hospital assumes legal responsibility for the patient medical information stored by each hospital, along with the EMR systems itself.
This means the first hospital is now managing multiple sets of records across two or three different EMR systems – meaning both different record sets AND different software. This also means licensing fees for multiple systems, along with management and upkeep of the records within the system and the systems themselves are all the responsibility of the acquiring hospital. This situation can occur even without acquisitions. The same matrix of inefficiency exists even when one hospital upgrades or changes over from a legacy system to a new EMR system.
Ultimately, this complicates growth and the merger/acquisition, or upgrade process through inefficiency. The integration point of these types of transitions is the best opportunity to address these inefficiencies and create real savings for the future. Luckily, for hospitals that find themselves facing such a situation, a solution exists.
The Solution

Partnering with Cariend for EMR System Needs
Partnering with a medical records custodian like Cariend gives your facility or hospital the opportunity to eliminate unnecessary acquired EMR systems, eliminate the risk of holding excess or unneeded records, and streamline health information management processes within a given organization. With years of experience navigating a variety of medical records management systems, the team at Cariend can offer a solution to your situation – no matter how complex.
The process starts with a review of your current EMR system processes and functions, with an experienced eye trained for finding inefficiencies. The team at Cariend can then provide a solution tailored to your facility’s specific health information management needs, helping you eliminate excess software fees and save on records storage and requests.
As your hospital or medical facility grows, consider the implications of such growth. Mergers and acquisitions are a new constant in the medical services landscape, so it may only be a matter of time before your hospital or facility experiences the constraints created by such growth. If reducing inefficiency in EMR systems at your hospital or medical facility is something you’re interested in, contact Cariend today to learn more.